Pain in the Lower Back during Pregnancy
Back pain during pregnancy isn’t surprising, but it still deserves attention. Pain in the lower back or discomfort is common during pregnancy and should be expected to some degree by most women. Back pain may be experienced during any point of your pregnancy; however, it most commonly occurs later in pregnancy as baby grows.
Back pain can disrupt your daily routine or interfere with a good night of sleep. The good news is there are steps you can take to manage the back pain that you experience
Causes of the lower back ache
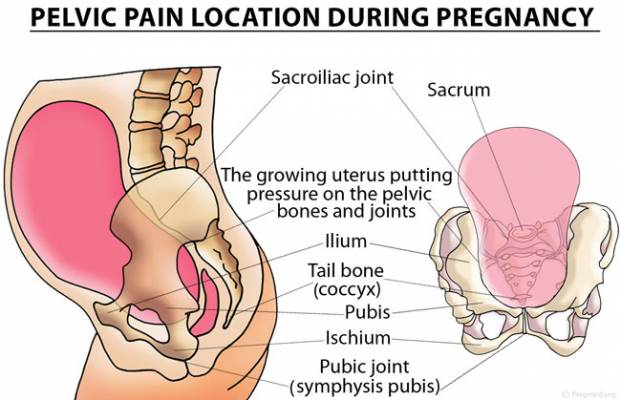
Image source – Pregnancy Health
There are many possible reasons why it happens. Here are some of the more likely causes:
-
Weight gain. During a healthy pregnancy, women typically gain between 25 and 35 pounds. The spine has to support that weight. That can cause lower back pain. The weight of the growing babyand uterus also puts pressure on the blood vessels and nerves in the pelvis and back.
-
Muscle separation.
The abdomen consists of two parallel bands of muscles that connect in the middle of the abdomen. These muscles help to stabilize the spine and support the back. During pregnancy, the growing fetus pushes against the abdominal muscles, causing them to stretch and, in some cases, separate. This pressure can result in a condition called diastasis recti. During the second and third trimesters, some women may develop a bulge or “pooch” in their stomach. This is a sign that their abdominal muscles are separating to allow room for the growing uterus. As the abdominal muscles stretch, they become weaker. This can increase a woman’s risk of injuring her back or developing low-back or pelvic pain.
-
Posture changes.
Pregnancy shifts your center of gravity. As a result, you may gradually — even without noticing — begin to adjust your posture and the way you move. This may result in back pain or strain.
-
Hormone changes.
During pregnancy, your body makes a hormone called relaxin that allows ligaments in the pelvic area to relax and the joints to become looser in preparation for the birth process. The same hormone can cause ligaments that support the spine to loosen, leading to instability and pain.
-
Muscle separation.
As the uterus expands, two parallel sheets of muscles (the rectal abdominis muscles), which run from the rib cage to the pubic bone, may separate along the center seam. This separation may worsen back pain.
-
Stress.
Emotional stress can cause muscle tension in the back, which may be felt as back pain or back spasms. You may find that you experience an increase in back pain during stressful periods of your pregnancy.
How to treat the pain?
Unless you had chronic backaches before you got pregnant, your pain will likely ease gradually before you give birth.
Meanwhile, there are many things you can do to treat low back pain or make it rarer and milder
-
Practice good posture
As your baby grows, your center of gravity shifts forward. To avoid falling forward, you might compensate by leaning back — which can strain the muscles in your lower back and contribute to back pain during pregnancy. Keep these principles of good posture in mind:
- Stand up straight and tall.
- Hold your chest high.
- Keep your shoulders back and relaxed.
- Don’t lock your knees.
When you stand, use a comfortably wide stance for the best support. If you must stand for long periods of time, rest one foot on a low step stool — and take time for frequent breaks.
Good posture also means sitting with care. Choose a chair that supports your back, or place a small pillow behind your lower back.
-
Get the right gear
Wear low-heeled — not flat — shoes with good arch support. Avoid high heels, which can further shift your balance forward and cause you to fall.
You might also consider wearing a maternity support belt. Although research on the effectiveness of maternity support belts is limited, some women find the additional support helpful.
-
Lift properly
When lifting a small object, squat down and lift with your legs. Don’t bend at the waist or lift with your back. It’s also important to know your limits. Ask for help if you need it.
-
Sleep on your side
Sleep on your side, not your back. Keep one or both knees bent. Consider using pregnancy or support pillows between your bent knees, under your abdomen and behind your back.
-
Try heat, cold or massage
While evidence to support their effectiveness is limited, massage or the application of a heating pad or ice pack to your back might help.
-
Include physical activity in your daily routine
Regular physical activity can keep your back strong and might relieve back pain during pregnancy. With your health care provider’s OK, try gentle activities — such as walking or water exercise. A physical therapist also can show you stretches and exercises that might help.
You might also stretch your lower back. Rest on your hands and knees with your head in line with your back. Pull in your stomach, rounding your back slightly. Hold for several seconds, then relax your stomach and back — keeping your back as flat as possible. Gradually work up to 10 repetitions. Ask your health care provider about other stretching exercises, too.
-
Consider complementary therapies
Some research suggests that acupuncture might relieve back pain during pregnancy. Chiropractic treatment might provide comfort for some women as well. However, further research is needed. If you’re considering a complementary therapy, discuss it with your health care provider. Be sure to tell the chiropractor or acupuncturist that you are pregnant.
When to see the doctor?
Women who experience back pain during pregnancy should contact their obstetrician or other healthcare providers if they experience the following symptoms:
- severe pain
- pain that lasts more than 2 weeks
- cramps that occur at regular intervals and gradually intensify
- difficulty or pain when urinating
- a tingling sensation in the limbs
- vaginal bleeding
- irregular vaginal discharge
- fever
Women who suffer from severe back pain that persists longer than 2 weeks should discuss treatment options with their healthcare provider.
Also read – Reasons of cramping during pregnancy













